10 Biggest Medical Scandals in History
By Matt Goddard, Top Masters In Public Health Degrees, 20 February 2013.
By Matt Goddard, Top Masters In Public Health Degrees, 20 February 2013.
When it comes to public health, there’s little margin for error. And when crises break out, the repercussions can be serious, not to say deadly, and linger long in the memory.
From genuine mistakes and media-fuelled hysteria, to wilful and even malicious deception, medical scandals and other health disasters can be truly devastating. It’s troubling to think that the companies and individuals people turn to when their wellbeing is at stake are far from infallible; indeed, some might even have more sinister agendas in mind.
While legislation and technological advances have helped to stamp out some of these threats, recent high-profile cases show that in the fiercely competitive and profits-driven pharmaceutical industry - and in the arena of public health more widely - these kinds of scandals remain a menace to society. Read on for the 10 biggest medical scandals in history.
10. MMR Vaccine Controversy - United Kingdom (1990s)
Claims about the MMR vaccine’s connection with autism made headlines in the UK in the late Nineties. In 1998, English surgeon and medical researcher Andrew Wakefield led a group that published a paper in highly-regarded medical journal The Lancet presenting evidence that linked the measles, mumps and rubella vaccine to developmental disorders. Wakefield’s claims brought about a number of major studies, none of which proved any such link. Yet the article had already incited a media frenzy and led to multi-million pound litigation proceedings. Concerns about the vaccination reached as far as the United States and Japan.
An inevitable consequence of the report was that MMR vaccination rates fell in the UK and Ireland, resulting in significant increases in cases of - and even deaths related to - mumps and measles. In 2004, an investigation by The Sunday Times journalist Brian Deer finally revealed that Wakefield had manipulated the evidence in his paper and also had various conflicts of interests that were not divulged.
Wakefield’s paper was finally fully withdrawn in 2010 - the same year in which he was struck from the General Medical Council. Scientific consensus now holds that there is no link between autism and the MMR vaccine.
9. Gurgaon Illegal Kidney Transplant Racket - India (2008)
In 2008, India was shocked when an illegal kidney transplant racket was exposed in the city of Gurgaon, in the state of Haryana. It was reported that hundreds of poor workers were intimidated at gunpoint or otherwise tricked into donating organs, and that authorities believed the recipients had been wealthy individuals - foreigners included.
It was revealed that, over a 10-year period, as many as 600 kidney transplants were performed in a private house that was fitted with high-tech operating equipment. After a January 2008 raid, police made several arrests and saved five unwitting donors, who were transferred to a nearby hospital. Astonishingly, it was later discovered that a minimum of two hospitals had been involved in the scheme.
It is thought that labourers were told there would be work available for them if they came to the house, only for them to be offered approximately 50,000 rupees ($1,250) for their kidneys. If they refused, the workers were drugged and their organs were forcibly removed - after which the organs were sold for up to 10 times the aforementioned price. Soon after the raid, some kidney recipients were detained, including three Greek citizens and a US-based Indian couple.
8. Jim the Horse Tetanus Scandal - United States (Early 1900s)
Jim the horse’s contribution to saving lives towards the end of the 19th century cannot be questioned. During his time, the onetime milk wagon horse was used to produce over seven gallons of serum that held antibodies used against diphtheria - the contagious and potentially deadly respiratory tract illness that’s especially dangerous to young children.
Then in early October 1901, Jim was found to have contracted tetanus and was put to sleep. At about the same time, a girl in St. Louis died, and it was discovered that the serum from Jim had caused her death. It was subsequently revealed that serum taken from the horse on September 30 onwards was infected with incubation-phase tetanus.
Damningly, the samples had not been tested - a process that could easily have uncovered the infection. Additionally, bottles of serum taken on September 30 had been marked “August 24.” Such oversights cost the lives of a further 12 children. The episode contributed in part to the passing of the United States Biologics Control Act of 1902 and paved the way for the introduction of the Food and Drug Administration (FDA) in 1906.
7. Heparin Adulteration - China (2008)
In 2008, the US Food and Drug Administration (FDA) announced a large-scale recall of heparin after discovering contaminated raw batches of the drug that had been manufactured in China by Scientific Protein Laboratories, a US firm. Heparin is injected into many people to prevent blood clots and is derived from slaughtered animal tissues such as pigs’ intestines and cows’ lungs.
The recall followed an alleged 81 deaths and 785 other reports of severe injuries linked to the drug. Investigations identified the contaminant as an over-sulphated derivative of chondroitin sulphate, which can be used as a dietary supplement, but not as a medicine. Worst of all, several compelling reasons led authorities to believe that the contamination was deliberate, including the fact that it imitates the effect of heparin yet is a fraction of the price.
The motive for the contamination is thought to have been a combination of cost cutting and a lack of the right kinds of pigs in China. By early 2012, the FDA had added 22 Chinese heparin ingredient suppliers to an import alert list. Worryingly, the FDA also stated that it does not have enough money and that it is not up to them to inspect such overseas manufacturers on a regular basis.
6. Elixir Sulphanilamide Mass Poisoning - United States (1937)
The United States Federal Food, Drug and Cosmetic Act (FDCA) came into effect in 1938. The act gave the FDA the power to oversee the safety of food, drugs and cosmetics. And in a way, the FDA as we know it today was born partially as a result of 1937 Elixir Sulphanilamide disaster - or at least the public outcry it sparked.
Over 100 people were poisoned and died when sulphanilamide, an antibiotic, was dissolved in diethylene glycol (DEG) and marketed as Elixir Sulphanilamide. Despite reports indicating that DEG was dangerous to humans, such information was not widely known about, and the chief pharmacist at drugs manufacturer S. E. Massengill Company was oblivious. At the time, there were no rules demanding safety testing of new medicines before they went on sale. And while drug companies routinely carried out animal testing, in this case Massengill hadn’t undertaken any.
Soon after the raspberry-flavoured elixir hit the market in September 1937, there were reports of deaths, and subsequent investigations isolated the cause. The scandal led to the passing of the FDCA, but the Massengill Company was only subject to a minimum fine due to the stipulations of the previous 1906 Pure Food and Drugs Act. Still, with his trial pending, the company’s chief pharmacist took his own life.
5. New England Compounding Centre Meningitis Outbreak - United States (2012)
In October 2012, the US Centres for Disease Control and Prevention (CDC) followed the trail of an outbreak of fungal meningitis back to the contamination of medication administered as epidural steroid injections. Packaged and sold by Massachusetts-based pharmacy the New England Compounding Centre (NECC), the spoiled drugs had been sent to 75 clinics, hospitals and surgeries across 23 states. Between May and September of that year, approximately 14,000 patients received the medication.
While people reported symptoms in August, the infection was so strange that a common cause was not suspected until the following month. In fact, cases of meningitis attributed to the fungal varieties implicated were so rare that their discovery and treatment explored new medical territory.
By mid-January 2013, 678 people had contracted the fungal disease and 44 had died. Preliminary investigations found dirty, unhygienic conditions at the NECC - including steroid solutions contaminated with fungus. Authorities discovered that the NECC had distributed orders of the drug despite the fact that they were still waiting for test results that would indicate whether or not the shipment was sterile. By December 15, 2012, over 400 litigation proceedings had been launched against NECC. As of February 2013, the scandal is still unfolding.
4. PIP Silicone Implant Scandal - France (2009)
Established in 1991, French company Poly Implant Prothèse (PIP) sold breast implants for nearly two decades. In its prime, PIP manufactured 100,000 implants a year, supplying an estimated total of 400,000 women across the globe. Then in 2009, French surgeons began to report unusually large numbers of implants that had ruptured.
The events that unfolded were dramatic. It was found that, in 2001, PIP had begun using unauthorized, industrial-grade silicone for most of their implants, rather than the medical-grade silicone they were supposed to. This reduced the expense of manufacturing the implants by 90 percent - but with another cost: there was an increased chance of ruptures, which could cause irritation, inflammation, and toxic substances to escape into the body. And while there has been no proven link as yet, cancer was discovered in 20 French women with implants alleged to have been defective.
After one diagnosis of anaplastic large-cell lymphoma, French authorities recommended that women with PIP implants have them removed. And out of 672 preventative removals registered by the health agency AFSSAPS, the implants had burst in 43 instances (as of December 2011). In other countries, the crisis left thousands of women fearful. The scandal prompted a wave of legal complaints that led to PIP’s bankruptcy in 2009 and eventual liquidation two years later.
3. Toxic Cough Syrup - Panama (2007)
In 2007, 70 years on from the infamous Elixir Sulphanilamide poisoning scandal in the US, a similar outbreak caused the tragic loss of hundreds of lives. In Panama, pharmaceutical manufacturers used diethylene glycol, which is commonly used in antifreeze and brake fluid, to make cough syrup, mistakenly believing it to be glycerine. The offending ingredient led to no less than 365 deaths in Panama and was traced back to China.
At first, the investigation was difficult, but eventually it was discovered that the imported diethylene glycol used in the medicine was originally named “TD glycerine,” which in China apparently indicates that it is a glycerine substitute. China denied responsibility for the scandal, as the name had been altered to “glycerine” upon the liquid’s arrival in Panama when one Aduanas Javier de Gracia filled out the customs declaration. However, The New York Times later found out that the Chinese manufacturer wasn’t even licensed to make pharmaceutical ingredients.
Moreover, this kind of contamination is not uncommon. In 2009, it was reported that 84 babies, if not more, had died in Nigeria after ingesting cough syrup also believed to have been contaminated with diethylene glycol. In a 1995 article in the British Medical Journal, American paediatrician Dr. Michael L. Bennish, who had been a key player in cracking the Panama case, estimated that such poisonings could be responsible for “tens of thousands” of deaths around the world.
2. HIV-Tainted Blood Scandal - Japan (1980s)
Japan did not have any official reports of HIV until 1985, four years after the first AIDS-like illness was identified in Los Angeles in 1981. In 1983, Japan’s Ministry of Health and Welfare was informed about a US licensed heat-treated blood product that could kill HIV. When overtures were made to license this product in Japan, the country’s chief provider of blood products, the Japanese Green Cross Corporation, strongly objected, stating that the product would provide unfair competition (as they refused to explore heat-treated alternatives).
The product was not taken up, and the Japanese Ministry of Health acted by ordering that untreated blood products be screened, by carrying out tests on heat-treating, and by encouraging the public to give blood. In the meantime, the Green Cross Corporation distributed safety guarantees regarding their unheated blood products to patients - a significant number of whom were afflicted with haemophilia - and the decision proved disastrous.
During this time period, it’s thought that up to 2,000 Japanese haemophiliac patients contracted HIV through tainted blood products. Prominent officials in Japan’s Ministry of Health and Welfare, a top haemophilia doctor and company executives were later indicted for involuntary manslaughter.
1. Thalidomide Birth Defects Scandal - Germany and Worldwide (1950s–1960s)
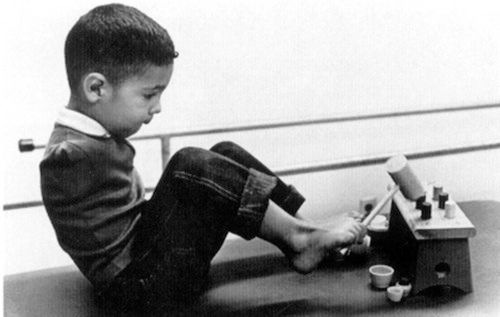
The thalidomide distribution scandal of the late 1950s and early 1960s left a lasting effect on the world. Released as a sedative drug in the late 1950s, thalidomide was also found to ease the effects of morning sickness. The drug was sold from 1957, but it was withdrawn in 1962, when it was discovered that it was capable of interfering with developing foetuses and causing birth defects.
Initially, thalidomide was held to be a “wonder drug.” At the time, the use of medication during pregnancy was not thoroughly regulated. Drugs were not properly tested for the possible danger they posed to babies in the womb. Back then, scientists didn’t even think that drugs taken by a pregnant woman could harm a growing foetus. Ultimately, thousands of pregnant women took thalidomide during its five years on the market - and the effects were horrendous.
Across 46 countries, over 10,000 children were born with defects like phocomelia. This disorder commonly results in abnormalities to the arms and legs, but it can also have an impact on other parts of the body. In the UK alone, around 2,000 babies were born with birth defects resulting from thalidomide; roughly 1,000 died inside a few months, while 466 of those affected were still alive in 2010. German company the Grünenthal Group, who created the drug, issued an apology in 2012, more than 50 years after the drug first went on sale.
Related Posts:










No comments:
Post a Comment
Please adhere to proper blog etiquette when posting your comments. This blog owner will exercise his absolution discretion in allowing or rejecting any comments that are deemed seditious, defamatory, libelous, racist, vulgar, insulting, and other remarks that exhibit similar characteristics. If you insist on using anonymous comments, please write your name or other IDs at the end of your message.